TOXICOLOGY (PART
I)
Mrs.
Ma. Indira P. Bio, RMT
TOXICOLOGY
l The basic
science of poisons
l The study of the
adverse effects of chemicals on living organisms
Different Areas of Toxicology:
Mechanistic
Descriptive
Regulatory
The Importance
of Dose
Poison - any agent capable of deleterious response in a biological system,
seriously injuring function or producing death
What
is there that is not poison? All things
are poison and nothing is without poison. Solely the dose determines that a
thing is not a poison
-Paracelsus
DOSE -
the total amount of a toxicant administered to an organism at a specific time
intervals.
- quantity per unit body weight or per
body surface area
There are no harmless substances, only harmless
ways of using substances
Emil Mrak
Major
factors that influence toxicity:
1.
Route & Site of Exposure
Major routes by which toxic agents
gain access to the body:
GI Tract
Lungs
Skin
Bloodstream
Other parenteral routes
2.
Duration & Frequency of Exposure
Acute - exposure to a
chemical for less than 24 hours
Subacute - repeated exposure
to a chemical for 1 month or less
Subchronic - 1-3 months
Chronic more than 3 months
Drugs of Abuse
l
Cocaine
l
Opiates
l
Methadone
l
Amphetamines
l
Benzodiazepines
l
Phencyclidine
l
Barbiturates
l
Marijuana
l
Lysergic
Acid Diethylamide (LSD)
COCAINE
History of
Cocaine Use
Cocaine
was first extracted from coca in the 19th century and was at first hailed as a
miracle drug, being the first ever discovered local anaesthetic.
In
1880s, it was freely prescribed for exhaustion, depression and morphine
addiction
Cocaine
was originally a vital ingredient in "Coca cola", hence the name, and
until its addictive characteristics were discovered, it remained in the drink.
Source
Derived
from the plants of Erythroxylon coca indigenous to Peru
and Bolivia
Chemistry
Cocaine
is benzoylmethylecgonine
An
ester of benzoic acid and a nitrogen base
Route of
administration
Inhalation
Effects
Induces
a euphoric state, hallucinatory states and violent behavior
Has
dopaminergic effects that induce increased calcium influxes in dopaminergic
neurons which activates phospholipases.
Treatment
Antidepressants,
including tricyclics and fluoxetine (Prozac)
Half-life of cocaine: 0.5-1 hour
Benzoylecgonine - the primary product of hepatic
metabolism which is eliminated in the
urine
- the presence of this metabolite in the urine is a
sensitive and specific indicator of cocaine use.
- can
be detected in the urine for up to 3 days after a single use
- in chronic heavy users it can be detected for up
to 20 days after the last dose.
Screening test: immunoassay
Confirmatory Test: GC with mass spectrometry
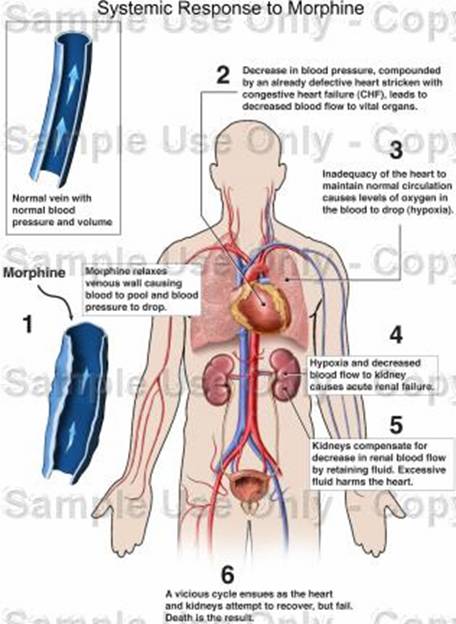
OPIATES
Morphine
Codeine
Heroin
Poppies
will make you sleep
-
Wizard of Oz
Source:
Papaver somniferum or poppy plant
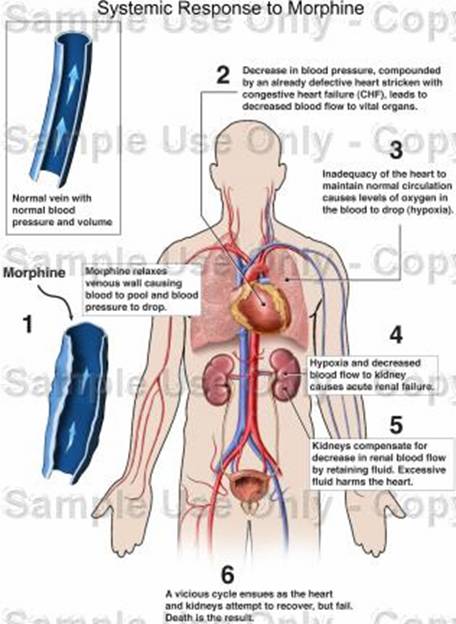
Morphine
Morphine is a
narcotic analgesic. Morphine was first isolated from opium in 1805 by a German
pharmacist, Wilhelm Sertürner. Sertürner described it as the Principium
Somniferum. He named it morphium - after Morpheus, the Greek god of dreams.
Route of Administration:
Morphine
can be taken orally in tablet form, and can also injected subcutaneously,
intramuscularly, or intravenously
Opiates share
the same brain receptors and have analgesic properties similar to the
naturally occurring painkillers in the body known as endorphins or enkephalins.
Their sensory and motor CNS depressant effects make them valuable clinically as
analgesics, sedatives and antispasmodics
Codeine
Also
known as methylmorphine or morphine monomethyl ether
Heroin
Derived
from the dried sap of the opium poppy.
Heroin
is in the same category of painkillers as morphine, its derivatives and
codeine.
The
effects of heroin include significant pain relief, but as dose is increased, euphoria
is produced.
At
very high doses, sedation, respiratory depression and coma may occur.
Route
of Administration
Intravenous
Addiction
to the drug is readily recognized by the presence of needle tracks on the
users arm and hands and by extensive thrombosis of the peripheral veins.
Major
metabolite of heroin: N-acetyl morphine
and morphine
Treatment:
Naloxone given intravenously
Methadone for chronic cases
Confirmatory
test: GC with spectrometry
Methadone
Introduced
into the United States
in 1947 as an analgesic (Dolophine),
A
non-bicyclic drug that binds competitively with morphine to m-
receptors in the brain.
Addictive
effects are less than those of equivalent concentrations of heroin
Methadone
is primarily used today for the treatment of narcotic addiction
Amphetamines
Amphetamines
belong to a group of drugs called psychostimulants that stimulate the central
nervous system.
Street
terms for methamphetamine: Meth, poor man's cocaine, crystal meth, ice, glass,
speed
Typically
meth is a white powder that easily dissolves in water
Amphetamine-like
substances that causes cross-reactions with amphetamine assays:
Adipex
Benzedrine
Preludin
Desoxyn
Didrex
Ritalin
Ionamin
Effects:
Exerts
symphathometic effects due to its uncanny resemblance to epinephrine and
norepineprine
They
have effects on the dopaminergic pathways causing psychic stimulation and
excitability leading to euphoric states and increase mental and physical
activity.
Route of Administration:
Most
commonly swallowed, injected (methamphetamine) or smoked. They are also snorted
, or sniffed , through the nose.
MDMA(Methylendioxymethylamphetamine)
Another
designer drug related to amphetamines. It is usually swallowed in the form of
small tablets, but is also sometimes injected.
- Similar (in nature) to other
amphetamines and hallucinogens
- It speeds up the nervous
system and acts as a mood enhancer.
Benzodiazepines
Also
referred to as minor tranquillisers.
They
work by slowing down the activity of the CNS.
They
slow the messages going to and from the brain to the body, including physical,
mental and emotional responses.
family
of drugs used to treat insomnia, anxiety, panic attacks, muscle spasms, and seizure
disorders.
Diazepam
(Valium) is the most prominent drug among these.
The
benzodiazepines act mainly through the GABA-A receptor subtype by potentiating
GABA transmission. GABA is a ubiquitous neurotransmitter, involved in the
majority of inhibitory synapses in the brain. Thus, GABA suppresses neural
firing, inhibiting or regulating other neurotransmitters including serotonin,
norepinephrine, and dopamine
Rohypnol
Also
known as "the date-rape drug".
A
tablet can be dropped into a victims drink causing them to become drowsy and to
lose their memory of any subsequent events.
Phencyclidine
- PCP (phencyclidine) was
originally developed in the 1950's by Parke, Davis & Company.
- Parke Davis marketed it for
a short amount of time as a surgical anesthetic for humans under the trade
name Sernyl, but it caused agitation, delusions, and terrifying hallucinations
in patients after surgery.
- Because of these side
effects, it was removed from the human market and sold to veterinarians
for surgery on animals under the trade name Sernylan.
- The commercial product
Sernylan(R) was withdrawn from the market in 1978.
Street Names:
angel
dust
Ozone
Wack
rocket
fuel
Killer
joints
crystal
supergrass
Snorted
Smoked
eaten
PCP
is classified as a dissociative
anesthetic
It
can act as a stimulant, a depressant, an analgesic (decreasing pain) or a
hallucinogen depending on the dose and route of administration.
In its pure form,
PCP is a white crystalline powder that readily dissolves in water
. It is available
as a liquid (PCP base dissolved most often in ether),
but typically it is sprayed onto leafy material such as marijuana,
mint,
oregano,
or parsley, and smoked.
Effects
PCP
affects multiple neurotransmitter systems in the brain. For example, PCP
inhibits the reuptake of dopamine, norepinephrine and serotonin and also
inhibits the action of glutamate by blocking receptors. Some types of opioid
receptors in the brain are also affected by PCP.
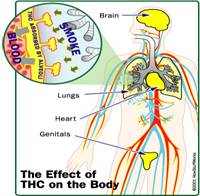
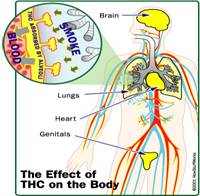
Marijuana
Cannabis
sativa
One
of the oldest and widely used of the mind altering drugs
It
is a mixture of cut, dried and ground portions of the hemp plant Cannabis
sativa
Hashish refers to a more potent product
produced by extraction of the resin from the plant
Route of administration:
Smoked
Oral
ingestion
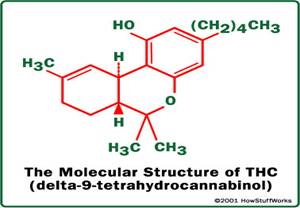
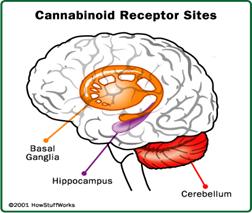
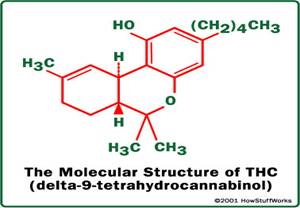
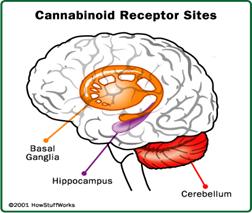
The principal
psychoactive agent in marijuana is delta-9 tetrahydrocannabinol (THC)
THC Molecule
THC
is a very potent cannabinoid chemical.
THC
mimics the actions of anandamide.
When
THC binds with cannabinoid receptors inside the hippocampus, it interfered with
the recollection of recent events.
An
IV dose of only one mg can produce serious mental and psychological effects.
Lysergic Acid Diethylamide (LSD)
A
semisynthetic indolakylamine and a hallucinogen
Can
be found in several others forms -- powder or crystal, liquid, gelatin squares,
laced on a sugar cube and capsules, or as a small pill.
Most
commonly sold in the form of blotter paper, which is small paper squares that
has been dipped in LSD.
TOXICOLOGY (PART II)
Route and Site
of Exposure:
Ingestion
(Gastrointestinal)
Inhalation
(Lungs)
Dermal
or Percutaneous (Skin)
Parenteral
Duration and
Frequency of Exposure:
Acute
exposure exposure to a chemical for less
than 24 hours
Subacute
repeated daily exposure for less than 1 month by a specific route
Subchronic
extends the daily exposure to 90 days or 3 months
Chronic
lifetime exposure
Dose-Response Relationship
characterizes
the correlation between exposure concentration and the spectrum of effects.
Toxicity Rating
System
Toxicity Rating Lethal Oral Dose in Ave. Adult
Super Toxic <5 mg/kg
Extremely Toxic 5-50 mg/kg
Very Toxic 50-500 mg/kg
Moderately Toxic 0.5-5 g/kg
Slightly Toxic 5-15 g/kg
Practically
Non-toxic >15 g/kg
Alcohol
The most
commonly abused substance
The
effects of alcohol may appear within 10 minutes after consumption; proportional
to its concentration in the blood.
Alcohol
intoxication is defined by blood alcohol concentration. BAC is defined as grams
of alcohol per deciliter of blood.
Alcohol
acts as a CNS depressant.
Effects:
0.05 produces
inhibition and facilitates social interaction
0.10 results in
slurred speech
0.20 euphoria
and motor impairment
0.30 confusion
0.40 stupor
0.50 coma
0.60 respiratory
paralysis and death
Major Metabolic
Pathway
alcohol O acetaldehyde O
dehydrogenase II dehydrogenase II
CH3-CH2-OH ® CH3-CH ® CH3-C (acetate)
(ethanol)
(acetaldehyde)
I
O
The
oxidation occurs chiefly in the liver
Between
90-98% of the ethanol that enters the body is completely oxidized
Oxidation
is relatively constant with time, and it is little increased by the raising the
concentration in the blood
In
the adult, the average rate at which ethanol can be metabolized is 120mg/kg per
hour, or about 30 ml (1oz.) in 3 hours.
Common
Indicators of Ethanol Abuse
Test Comments
GGT Increases can
be seen before the onset of pathologic consequences
AST Increases occur
in conjunction with ethanol- related diseases
AST/ALT ratio A ratio of greater than 2.0 is highly
specific for
ethanol related diseases
HDL High serum HDL
is very specific for ethanol consumption
MCV Increased
erythrocyte MCV is commonly seen with excessive ethanol
consumption
Reference:
Clinical Chemistry
Bishop, Duben Engelkirk, Fody
Widmanns Clinical Interpretation of Laboratory
Tests
Sacher, McPherson
The Pharmacological Basis of Therapeutics (8th ed,
Vol. 2)
Gilman, Rall
TOXICOLOGY (PART III)
Note from editor: This one seems unfinished to me
But Ill be including this anyway. ^_^
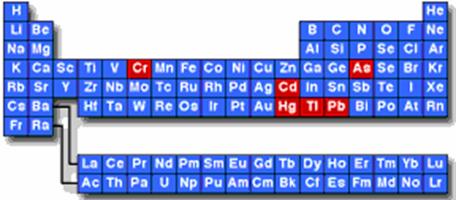
Heavy Metals
Mercury
Classification:
Inorganic mercury: elemental
mercury
mercury salts
Organic mercury: ethylmercury/methylmercury/phenylmercury
Physical/Chemical
Properties:
® Odorless, shiny,
silvery liquid; non-flammable; produces poisonous gas in fire
® Combines readily
with S, Cl, or O2 to form inorganic mercury.
® Binds with C to
form organic mercury
Hazards:
® Vapor pressure
is high
® Passes into the
brain and interferes with brain development
® Rapidly crosses
the placenta
Toxic Dose: 10-42 mg/kg
Toxidromes:
® Inhalation
® Subcutaneous/Intramuscular
Injection
® Dermal
® Ingestion
Specimen and
Examinations for Diagnosis
® Whole blood for
mercury levels
Biological limits: <
1 mcg/dL (inorganic mercury)
< 1 mcg/dL (methylmercury)
® 24-hour urine
for mercury levels
Biological limits: <
5 mcg/g creatinine (inorganic mercury)
® Hair for mercury
levels
Segmental
hair analysis (1 cm each) is useful in determining exposure or uptake of
mercury through diet. Not a good biomarker for inorganic mercury exposure